| Journal of Food Bioactives, ISSN 2637-8752 print, 2637-8779 online |
| Journal website www.isnff-jfb.com |
Review
Volume 5, March 2019, pages 43-56
The role of rutin and diosmin, two citrus polyhydroxyflavones in disease prevention and treatment
Alexander Gosslaua, b, *, Chi-Tang Hob, Shiming Lib
aDepartment of Science (Biology), City University of New York, BMCC, 199 Chambers Street, New York, NY 10007, USA
bDepartment of Food Science, Rutgers University, 65 Dudley Road, New Brunswick, New Jersey 08901-8520, USA
*Corresponding author: Alexander Gosslau, Department of Science (Biology), City University of New York, BMCC, 199 Chambers Street, New York, NY 10007, USA
DOI: 10.31665/JFB.2019.5177
Received: February 11, 2019
Revised received & accepted: March 11, 2019
| Abstract | ▴Top |
Chronic inflammation and dysregulation of apoptotic pathways leading to free radical-induced tissue damage are widely recognized as major underlying causes of major degenerative diseases, including cancer, diabetes, neurological and cardiovascular disorders. Citrus fruits are rich sources of polyphenolic flavonoids well known for their wide range of pharmacological properties. Rutin (quercetin-3-O-rutinoside) and diosmin (diosmetin 7-O-rutinoside) are two major polyhydroxyflavone glycosides abundantly found in citrus peels and, to a lesser extent, in pulp of a variety of different citrus species. During digestion, hydrolysis by intestinal enzymes and gut microbiota lead to the release of their corresponding bioactive aglycones (e.g., quercetin or diosmetin). Data obtained in cell-based, animal and clinical studies demonstrated strong preventive and/or therapeutic effects of rutin and its aglycone flavone quercetin. Although lesser studies available, our recent literature review suggests diosmin as promising citrus fruit polyhydroxyflavonoids, effective against various diseases associated with chronic inflammation.
Keywords: Citrus polyhydroxyflavones; Rutin; Diosmin; Chronic inflammation; Degenerative diseases
| 1. Therapeutic effects of citrus fruit polyphenolic flavonoids against degenerative diseases | ▴Top |
Chronic inflammation is widely recognized as a major underlying cause of various degenerative diseases. The accumulation of free radicals such as reactive oxygen species (ROS) or reactive nitrogen species (RNS) and inflammatory mediators (e.g. NO, prostaglandins, leukotrienes, thromboxanes) generated by immunocompetent leukocytes (e.g. macrophages and eosinophiles) is responsible for damaging effects on cells, tissues and organs (Aggarwal et al., 2012; Gosslau et al., 2011; Ley, 2001; Liu et al., 2018; Robbins et al., 2010; Roberts et al., 2009). It is generally believed that during severe chronic inflammation, accumulation of cell destruction is caused by these electrophilic species which oxidize—and thus damage—virtually all macromolecular compounds of the cell. Moreover, an activation by proteolytic metalloproteinases is coupled to even more cell damage leading to pathological conditions of various degenerative diseases (Aggarwal et al., 2012; Coussens and Werb, 2002; Kundu and Surh, 2008; Ley, 2001; Robbins et al., 2010). The antioxidative capacity of flavonoids is well documented to be effective on different layers such as radical scavenging, metal ion chelating, replenishing of endogenous antioxidant enzymes, inhibition of free radical generating enzymes as well as preventive and inhibitory effects on lipid peroxidation, DNA damage and protein modification caused by free radicals (Barreca et al., 2017; Panche et al., 2016; Tripoli et al., 2007).
Activation of NFκB plays a central role to initiate and promote the inflammatory response (Baud and Karin, 2009; Karin et al., 2002). The impact of chronic inflammation in carcinogenesis is well established (Coussens and Werb, 2002; Kundu and Surh, 2008; Liu et al., 2018). For a variety of different flavonoids, an inhibition of NFκB signaling via IKK to decrease iκB phosphorylation has been reported (Baud and Karin, 2009; Mena et al., 2014; Panche et al., 2016; Prasad et al., 2010; Spagnuolo et al., 2018). Other major pathways reported to be suppressed by flavonoids, thus decreasing inflammation, include mitogen activated protein kinases (MAPK), peroxisome proliferator-activated receptors (PPAR), c-Jun N-terminal kinase (JNK) and p38 (Hasan et al., 2017; Liu et al., 2017; Panche et al., 2016; Spagnuolo et al., 2018). Our studies have shown significant anti-inflammatory effects of flavonoid-enriched orange peel extracts as validated in cell-based and in vivo models for inflammation (Gosslau et al., 2014; Gosslau et al., 2011; Gosslau et al., 2018; Lai et al., 2015; Li et al., 2007; Sergeev et al., 2007; Wang et al., 2016). Chronic inflammation is also a key pathologic link between obesity and type 2 diabetes (T2D). The accumulation of free radicals released by immunocompetent cells, or derived from conditions of hyperglycemia and dyslipidemia, are responsible for progression of T2D. In a vicious cycle, more reactive radicals formed by high glucose expedite an impairment of the insulin receptor, causing a further disconnection of the insulin cascade, thus leading to chronic hyperglycemia and insulin resistance (Bluher, 2016; Boutens and Stienstra, 2016; Calle and Fernandez, 2012; Chawla et al., 2011; Donath, 2014). Antidiabetic effects of flavonoids are well documented to be based on biological activities against obesity, hyperglycemia, dyslipidemia and inflammation as extensively reviewed (Babu et al., 2013; Chen et al., 2016b; Leiherer et al., 2013).
The loss of essential cells in postmitotic tissues due to enhanced apoptosis play an important role in cardiovascular and neurological diseases (Loh et al., 2006; Moe and Marin-Garcia, 2016). Besides their inhibitory impact on the inflammatory cascade, therapeutic effects of flavonoids against cardiovascular and neurological disorders are believed to be based on suppression of apoptotic pathways, thus protecting endothelial, myocardial and nervous tissue (Barreca et al., 2017; Kumar and Pandey, 2013; Panche et al., 2016; Spagnuolo et al., 2018; Wang et al., 2018). For many cancers, on the other hand, an activation of apoptotic signaling can be considered as a pro-active self-defense mechanism of a living organism to weed out dysfunctional cells such as the precursors of metastatic cancer cells without creating secondary oxidative stress due to inflammation (Gosslau and Chen, 2004; Hassan et al., 2014; Wong, 2011). Activation of apoptotic signaling pathways by flavonoids, either intrinsically mediated by mitochondria or extrinsically via receptors are well documented and reviewed elsewhere (Meiyanto et al., 2012; Panche et al., 2016; Sharma et al., 2017). A crosstalk between apoptotic and inflammatory pathways is indicated by several studies which demonstrated that inhibition of NFκB signaling correlated with an induction of apoptosis (Nakano et al., 2006; Oeckinghaus et al., 2011). The anti-apoptotic role of NFκB in carcinogenesis is apparent by a hyperactivity of NFκB observed in certain type of cancers (Baud and Karin, 2009; Karin et al., 2002). In fact, the inhibition of NFκB signaling by many flavonoids is in accordance with their proapoptotic effects demonstrating the close link between oxidative stress, chronic inflammation, and cancer. In accordance to its anti-inflammatory and antioxidant effects as well as their capacity to modulate apoptotic pathways, several studies have demonstrated the effects of citrus flavonoids against diseases related to chronic inflammation such as cardiovascular, neurological and immunological disorders, diabetes, arthritis and different cancers which have been extensively reviewed elsewhere (Barreca et al., 2017; Kumar and Pandey, 2013; Panche et al., 2016; Prasad et al., 2010; Spagnuolo et al., 2018; Wang et al., 2018).
Flavonoids comprise a large group of natural compounds with variable structures commonly found in pulp and peel of different citrus fruits. Citrus plants belong to the family of Rutaceae which comprises many species such as citrus sinensis (sweet orange), citrus aurantium (sour oranges), citrus reticulata (mandarin), citrus limon (lemon), citrus medica (citron), citrus aurantifolia (lime) and citrus paradisi (grapefruit). In citrus fruits, the inner layer of the pericarp (e.g., meso- and endocarp) contains a multitude of juice sacs, as major site for flavonoid synthesis. When the distal part enlarges, it will break down and fill edible pulp with liquid, the juice of citrus fruits which contains a variety of different flavonoids (Garcia-Luis et al., 2001; Iglesias et al., 2007; Kimball, 1999). In 1930, the first flavonoid, later characterized as rutin, was isolated from oranges (Kumar and Pandey, 2013). Since then, many more flavonoids were identified and characterized as bioactive compounds in peels and juice of citrus fruits (Gattuso et al., 2007; Meiyanto et al., 2012; Nair et al., 2018; Nogata et al., 2006; Putnik et al., 2017). In citrus fruits, polyhydroxylated flavonoids (PHFs) and polymethoxylated flavonoids (PMFs) are considered as major bioactives (Barreca et al., 2017; Lai et al., 2015; Li et al., 2009; Zhao et al., 2018). It is generally believed that antioxidant and anti-inflammatory activities are the main underlying mechanisms for the health-promoting effects of PHFs and PMFs. In light of the beneficial effects of PHFs and PMFs as main bioactives of citrus fruits, we noted strong effects of hydroxylated PMFs (OH-PMFs) against disorders related to chronic inflammation such as diabetes and cancer (Gosslau et al., 2011; Gosslau et al., 2018; Lai et al., 2011).
Both rutin and diosmin are naturally occurring as flavone glycosides. Their aglycone moiety (e.g., quercetin for rutin and diosmetin for diosmin) is covalently linked via an O-glycosidic bond to their corresponding disaccharide (rutinose). Several reports have highlighted the structure-activity relationship of O-glycosylation on bioactivity. For rutin and diosmin, but also other flavonoid glycosides, it had been demonstrated that O-glycosylation reduces most bioactivities of their corresponding aglycones (Kumar and Pandey, 2013; Rice-Evans et al., 1996; Wang et al., 2018; Xiao, 2017). Usually, high amounts of rutin and diosmin are found in citrus peel and to a lesser extent in fruit juice (Kumar and Pandey, 2013; Li et al., 2009; Manthey and Grohmann, 2001; Panche et al., 2016; Wang et al., 2018). A comparison throughout different citrus species revealed a big difference of their contents in peels or juice (Gattuso et al., 2007; Nogata et al., 2006). Due to their covalent bond but also their lipophilic nature, the aglycone moiety (e.g., quercetin and diosmetin) occurs less frequently in citrus juice. Pharmacokinetic studies demonstrated that respective aglycones (e.g., quercetin and diosmetin) are responsible for strong bioactivity of rutin and diosmin. In fact, most studies on glycoside flavonoids revealed a strong bioactivity of their aglycones. It is well documented that rutin and diosmin are metabolized in the intestinal tract by β-glucosidases derived from intestinal cells and microbiota with a high absorption rate of the aglycones and their corresponding sugars (Hostetler et al., 2017; Marin et al., 2015). Quercetin has an impressive pleiotropic pharmacological profile, on levels of free radical-scavenging, antioxidant, anti-inflammatory, antiproliferative and modulatory bioactivities on apoptosis without showing severe side effects. After absorption, the liver is a major site for biotransformation to produce glucuronidated, sulfated, and methylated metabolites through mechanisms of phase II enzymes and bacterial enzymes from gut microbiota (Shahidi and Peng, 2018). Also for diosmin, it is well established that diosmetin represents the bioactive aglycone responsible for a variety of therapeutic effects. However, certain types of biological benefits have been demonstrated for some flavonoid glycosides (Kumar and Pandey, 2013; Rice-Evans et al., 1996; Wang et al., 2018; Xiao, 2017). A large number of studies have demonstrated the therapeutic effects of rutin and its aglycone quercetin (6267 and 17109 publications in PubMed as of February 2019 when searching for “rutin” or “quercetin”, respectively). In comparison, a lesser number of studies have been performed for diosmin and diosmetin (516 or 269 publications in PubMed for “diosmin” and “diosmetin”, respectively). Nonetheless, recent studies and knowledge gained by therapeutic application of a micronized purified flavonoid fraction ((Daflon®), a combination of 90% diosmin and 10% hesperidin) revealed a strong therapeutic potential for diosmin in a variety of disorders related to chronic inflammation.
| 2. Chemistry of polyhydroxyflavones (PHFs) | ▴Top |
Flavonoids represent the most common and widely distributed polyphenolic group comprised of more than 6000 compounds (Barreca et al., 2017; Kumar and Pandey, 2013; Panche et al., 2016; Wang et al., 2018). A common feature of flavonoids is the phenylbenzopyrone structure, two benzene rings joined by a linear three carbon chain (C6-C3-C6). They are categorized according to the saturation level of the central pyran ring and the existence of 3-OH group, mainly into flavones, flavanols, isoflavones, flavonols, flavanones, and flavanonols. Polyhydroxylated (PHFs) and polymethoxylated flavonoids (PMFs) are considered as major bioactives in citrus fruits (Barreca et al., 2017; Lai et al., 2015; Li et al., 2009; Zhao et al., 2018).
Polyhydroxyflavonoids are typical flavonoids in conventional concept, i.e. a core skeleton of C6-C3-C6 chrome with one or more hydroxyl groups on the ring, particularly on the A-ring and B-ring. These hydroxyl groups have net electron donating capacity to conjugated flavones or to the A-ring of a flavanone core. Electron donating property enables the strong and effective antioxidant activity of flavonoids, a subclass of polyphenols. At the initial stage, a quinone is formed after the oxidation of a polyphenol. Flavonoids are also effective radical scavengers because their stabilized conjugation system can catch reactive radicals and form relatively stable and less detrimental radicals. Hence, flavonoids or other polyphenols are the first line of the defense system against detrimental in vivo oxidizers and/or reactive radicals. Flavones are characterized by a double-bond in the ring structure between C-2 and C-3. Two major flavones found in citrus fruits are rutin and diosmin (Figure 1). Both are naturally occurring as flavone glycosides. Via an O-glycosidic bond, their aglycone moiety (e.g., quercetin for rutin and diosmetin for diosmin) is covalently linked to their corresponding disaccharide rutinose. The chemical structures of the two citrus flavonoids and their aglycones covered in this review are illustrated in Figure 1.
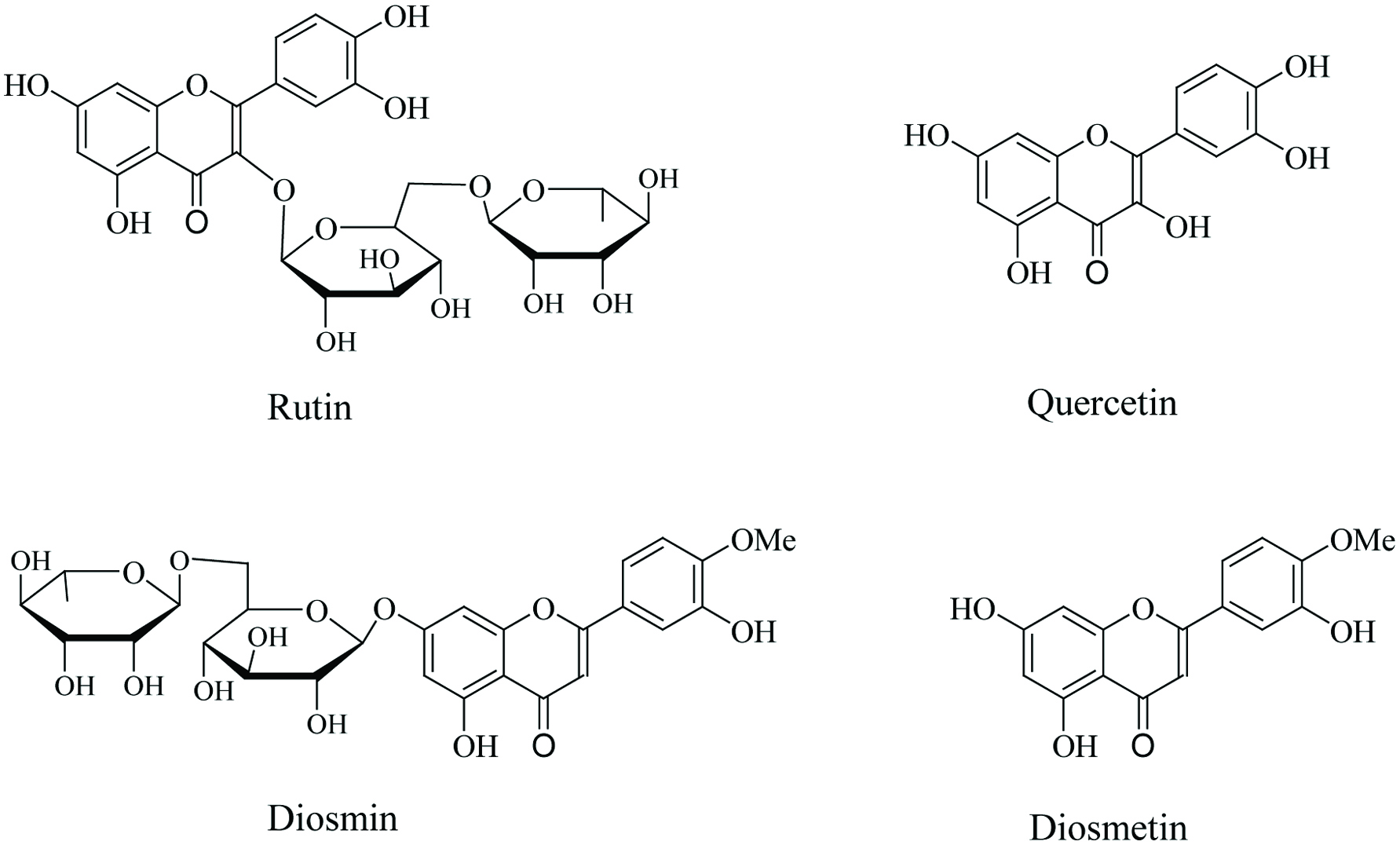 Click for large image | Figure 1. Chemical structures of rutin and diosmin and their aglycones. |
| 3. Bioactivity of glycosylated PHFs derived from citrus fruits and their corresponding aglycones | ▴Top |
3.1. Rutin and quercetin
Rutin (quercetin-3-O-rutinoside) represents the glycoside of the flavone quercetin (2-(3,4-dihydroxyphenyl)-3,5,7-trihydroxy-4-chromen-4-one) linked via 3-O glycosidic bond to the disaccharide rutinose (rhamnose-glucose) (Figure 1). Rutin occurs naturally in high amounts in peels of different citrus fruits species, whereas the amount in citrus juice is usually lesser. A comparative study throughout major citrus fruits revealed the occurrence of rutin only in juice of Citrus paradisi (Gattuso et al., 2007). A larger study which encompassed 42 species of the Citrus genus showed specific differences in amount and occurrence of rutin in different parts of the fruits depending on the species (Nogata et al., 2006). Early studies showed that both quercetin and rutin can attach to and traverse the small intestine of rats and humans with higher absorption rates for quercetin as compared to rutin (Carbonaro and Grant, 2005; Erlund et al., 2000; Manach et al., 1997). Pharmacokinetic studies demonstrated that rutin is deglycosylated to release the aglycone quercetin (Figure 1) by enzymatic hydrolysis upon entering the digestive tract by actions of intracellular β-glucosidases released from intestinal cells. Thereafter, quercetin undergoes biotransformation reactions to form glucuronidated, sulfated, and methylated metabolites through mechanisms of phase II enzymes but also enzymes from gut microbiota (Amaretti et al., 2015; Carbonaro and Grant, 2005; Erlund et al., 2000; Manach et al., 1997; Massi et al., 2017).
Among polyphenols, quercetin is considered to be one of the most potent bioactives found in plants. In excellent reviews, the impressive pharmacological profile of quercetin has been presented. The bioactivities of quercetin are pleiotropic on levels of free radical-scavenging, antioxidant, anti-inflammatory, antiproliferative and modulation of apoptosis without having severe side effects. It is generally accepted that antioxidant and anti-inflammatory effects are the underlying basis for most of chemopreventive and therapeutic effects of quercetin against degenerative diseases as demonstrated in a vast of cell-based in vitro, animal in vivo and human clinical settings (Cai et al., 2013; Gupta et al., 2016; Massi et al., 2017; Rani et al., 2015; Wang et al., 2018) (See Table 1 for anti-disease effects of quercetin and rutin). Anti-inflammatory effects of quercetin have been shown to systemically modulate various signaling pathways in the inflammatory cascade. A main target of quercetin include NFκB signaling on level of interference with IKK to decrease iκB phosphorylation (Chen et al., 2005; Cho et al., 2003; Granado-Serrano et al., 2012). Other pathways leading to anti-inflammatory activities of quercetin were demonstrated to be regulated through reduced activation of extracellular signal-regulated kinases (ERK) and p38 mitogen-activated protein kinase (MAPK) and/or signal transducer and activator of transcription 1 (STAT-1) (Ahn et al., 2008; Chen et al., 2005; Cho et al., 2003; Min et al., 2007). Suppression of the inflammatory cascade and subsequent lesser free radical induced cell damage are believed to be one of the major underlying molecular mechanisms of quercetin against cancer. The impact of chronic inflammation in carcinogenesis is well established and strong anti-cancer effects of quercetin are reflected by as many as 2700 publications in PubMed as of February 2019 when combining “quercetin and cancer” in searches and reviewed elsewhere (Gibellini et al., 2011; Haque et al., 2017; Kashyap et al., 2016; Khan et al., 2016; Nam et al., 2016). Besides strong anti-inflammatory bioactivities, proapoptotic effects of quercetin are conceivably the basis for chemoprotective and/or therapeutic effects in different cancers. The activation of apoptotic pathways by quercetin in various cancers during different cell cycle stages has been documented in vitro as well as in vivo (Gibellini et al., 2011; Granado-Serrano et al., 2010; Haque et al., 2017; Lee et al., 2010). For adenocarcinoma, breast, colon, lung and myeloid cancer, it has been demonstrated that apoptotic signaling by quercetin is triggered via caspase-3 activation through mechanisms of the mitochondrial-mediated pathway (Chien et al., 2009; Han and Zhang, 2016; Lee et al., 2015; Srivastava et al., 2016; Volate et al., 2005; Yang et al., 2006). Intriguingly, it has also been demonstrated that quercetin can differentially induce apoptosis in some cancer cells, but not in their normal counterparts (Gosslau and Chen, 2004; Lugli et al., 2009; Matsuo et al., 2005). As recently reviewed, epidemiological studies report that intake of quercetin-rich food significantly reduced the risk of gastric, colon and lung cancer by 43, 32 or 51%, respectively. Noteworthy, quercetin can alleviate severe side effects and thus potentiate the efficacy of anti-cancer drugs (Haque et al., 2017).
 Click to view | Table 1. Studies on anti-disease effects of rutin and diosmin and their aglycones quercetin and diosmetin |
The beneficial role of quercetin against cardiovascular problems is also well documented. In contrast to cancer where proapoptotic effects are considered to be beneficial, cardiovascular protection by quercetin appears to be mediated by inhibition of apoptotic pathways and repair of endothelial cells and cardiomyoctes (Chen et al., 2013b; Dayoub et al., 2013; Jagtap et al., 2009). Protective effects of quercetin against free-radical induced endothelial cell damage and apoptosis leading to atherosclerosis had been shown to be based on inhibitory effects on NO-guanylyl cyclase signaling (Perez-Vizcaino et al., 2006). Quercetin also showed protective effects against neurological disorders such as Alzheimer’s, Parkinson’s and Huntington’s disease as reviewed, recently (Budzynska et al., 2017; Costa et al., 2016; de Andrade Teles et al., 2018; Omar et al., 2017). The understanding of molecular mechanisms leading to these neurodegenerative diseases is still poor, but in addition to anti-inflammatory activities, a suppression of apoptotic signaling in nervous tissue, either mitochondria- or receptor-mediated were demonstrated to be one of the main underlying neuroprotective mechanisms exerted by quercetin (Ansari et al., 2009; Sharma et al., 2016; Zhang et al., 2015). Anti-apoptotic effects were reported to be triggered via suppression of Bax and/or activation of Sirtuin-1 signaling (Costa et al., 2016; Suganthy et al., 2016). Accordingly, quercetin induced inhibition of NFκB and STAT-1 pathways responsible for attenuation of neuroinflammation (Budzynska et al., 2017; Chen et al., 2005; Suganthy et al., 2016). In addition, quercetin stimulated NRF-2 dependent antioxidant responsive elements (NRF2-ARE) as cellular antioxidative defense system. Additional neuroprotective effects of quercetin may include activation of AMP-activated protein kinase (AMPK) signaling (Chen et al., 2016a; Wang et al., 2014). In various models of neuronal injury and neurodegenerative diseases, it had been demonstrated that quercetin reversed cognitive impairment and improved learning performance. These effects by quercetin might be attributed to a destabilization and clearance of β-amyloid peptides and hyperphosphorlyated tau, as demonstrated in animal models for Alzheimer’s disease (de Andrade Teles et al., 2018; Sabogal-Guaqueta et al., 2015; Suganthy et al., 2016).
It is well established that low-grade inflammation in adipose tissue leading to impairment of insulin signaling is a major cause in type 2 diabetes (Bluher, 2016; Boutens and Stienstra, 2016; Calle and Fernandez, 2012; Chawla et al., 2011; Donath, 2014; Goldfine et al., 2011). In different models for diabetes, quercetin showed strong anti-diabetic bioactivities in a metformin-like manner with increased insulin sensitivity and reduced hyperglycemia and hyperlipidemia (Chen et al., 2016b; Jeong et al., 2012; Jung et al., 2013; Yan et al., 2015). Additional anti-inflammatory and anti-obesity effects of quercetin contribute to effects against diabetes (Chen et al., 2016b; Leiherer et al., 2013). In the 3T3 preadipocyte model, an inhibition of NFκB signaling corresponded to a suppression of adipogenesis by quercetin-induced apoptosis, mediated through decreased phosphorylation of extracellular signal-regulated kinase (ERK) and c-Jun N-terminal kinase (JNK) (Ahn et al., 2008). These studies are in agreement with our recent study which showed strong anti-inflammatory effects of an orange peel extract enriched with flavonoids in an obese rat model for type 2 diabetes (Gosslau et al., 2018).
Although to a lesser extent as compared to quercetin, several studies also showed preventive and therapeutic effects of rutin against cancer, diabetes, cardiovascular, and neurological disorders. This is in support of pharmacological studies demonstrating intestinal hydrolysis of rutin to quercetin showing strong antioxidant, anti-inflammatory and differential regulation of apoptotic pathways as described above. Besides inhibitory effects on the inflammatory cascade, an induction of proapoptotic pathways in cancer cells were demonstrated to be responsible for anti-cancer effects of rutin (Perk et al., 2014; Sharma et al., 2013). In animal and cell-based models, proapoptotic effects of rutin in neuroblastoma, colon, lung, breast and prostate cancers were shown (Chen et al., 2013a; Guon and Chung, 2016; Saleh et al., 2019; Wu et al., 2017; Yang et al., 2000). As observed for quercetin, neuroprotective effects of rutin had been demonstrated in various models including Alzheimer’s, Parkinson’s and Huntington’s disease which had been reviewed, recently (Budzynska et al., 2017; Enogieru et al., 2018). In different rodent and cell models for Alzheimer’s disease, rutin prevented cognitive deficits by decreasing neuroinflammation and apoptotic cell death in nervous tissue (Javed et al., 2012; Park et al., 2014; Ramalingayya et al., 2017; Wang et al., 2012; Xu et al., 2014). Neuroprotective effects of rutin has also been demonstrated in a rat model for Huntington’s disease (Suganya and Sumathi, 2017) and a cell-based model for Parkinson’s disease (Magalingam et al., 2015). Beneficial effects of rutin against cardiovascular diseases are reflected by lipid-lowering bioactivities and effects against inflammation, atherosclerosis and apoptosis (Gong et al., 2010; Kanashiro et al., 2009; Salvamani et al., 2014; Santos et al., 1999; Wang et al., 2015). Furthermore, the biological effects of quercetin against diabetes correspond with studies on rutin which showed effects against hyperglycemia- and dyslipidemia as well as inflammation in adipose tissue (Ghorbani, 2017; Hsu et al., 2009; Wang et al., 2015).
3.2. Diosmin and diosmetin
Diosmin (diosmetin 7-O-rutinoside) (Figure 1) was first isolated from leaves of Scrophularia nodosa L., (Scrophulariaceae) in 1925. Later studies revealed that diosmin occurred abundantly in the pericarp (Bogucka-Kocka et al., 2013; Patel et al., 2013; Singhal et al., 2017; Yao et al., 2018) but also in the pulp and juice of different citrus fruits species (e.g., Citrus sinensis, C. clementina, C. aurantium, C. limon, C. aurantifolia and C. bergamia (Gattuso et al., 2007). A comparative study analyzing 42 Citrus species showed specific differences in levels of diosmin in pericarp, pulp and juice throughout the different species. However, for most of the species analyzed, the amount and occurrence of diosmin were higher in peel as compared to juice (Nogata et al., 2006). Diosmetin (3′, 5, 7-trihydroxy-4′-methoxyflavone) represents the aglycone part of diosmin linked via 7-O-glycosidic bondage to rutinose (Figure 1). It should be noted that diosmetin contains one methoxy group in addition to the three hydroxyl groups. In comparison, the quercetin molecule contains five hydroxyl groups without any methoxy group (Figure 1). Pharmacokinetic studies demonstrated that diosmin was rapidly absorbed, followed by hydrolysis through intestinal enzymes to release the aglycone diosmetin after an oral administration of diosmin (Cova et al., 1992; Silvestro et al., 2013). Diosmetin is then rapidly absorbed with a half-life in plasma ranging from 26 to 43 hours in humans (Cova et al., 1992). In accordance, cell-based experiments demonstrated high permeation rates and strong antioxidative bioactivities for diosmetin in contrast to diosmin (Serra et al., 2008; Villa et al., 1992). After intestinal absorption and biotransformation, metabolites are eliminated in the urine, mainly as glucuronic acid conjugates. Diosmetin-3-O-glucuronide was identified as the major circulating metabolite of diosmetin in plasma and in urine (Silvestro et al., 2013).
As compared to rutin and quercetin, lesser scientific research has been conducted on diosmin, but in several cell-based, animal and clinical settings, a wide range of biological activities were demonstrated for diosmin or diosmetin (Dumon et al., 1994; Feldo et al., 2018; Hasan et al., 2017; Senthamizhselvan et al., 2014; Shalkami et al., 2018; Silambarasan and Raja, 2012) (See Table 1 for anti-disease effects of diosmin and diosmetin). Most of the bioactivities of diosmin are based on strong antioxidant effects on levels of free radical scavenger activity to reduce oxidative stress. Strong anti-inflammatory effects of diosmin (or diosmetin) were demonstrated by suppression of proinflammatory cytokines and mediators (e.g., TNF-α, IL-1β, IL-6, IL-17, iNOS and COX-2) (Imam et al., 2015; Shalkami et al., 2018; Yu et al., 2014). The suppression of the inflammatory cascade by diosmin is based, at least in part, via inhibition of NFκB signaling (Shalkami et al., 2018; Yu et al., 2014). It was demonstrated that diosmin attenuated the canonical NFκB pathway on levels of IκB kinase (IKK) to decrease IκB-α phosphorylation (Imam et al., 2015). Another pathway affected by diosmin to alleviate oxidative stress and inflammation may include stimulation of the PPAR-γ pathway as demonstrated in a radiation-induced hepatic fibrosis rat model (Hasan et al., 2017).
Several studies have demonstrated that, due to its free radical scavenging and anti-inflammatory effects, diosmin exhibits therapeutic effects against cardiovascular disorders. A reduction of oxidative stress and apoptotic cell death in endothelial cells and cardiomyocytes has been shown (Bogucka-Kocka et al., 2013; Senthamizhselvan et al., 2014; Silambarasan and Raja, 2012). In epithelial cells, it was demonstrated that diosmin suppressed oxidative damage and subsequent apoptosis in a dose dependent manner via a decrease of the Bax/Bcl-2 ratio, cytochrome c release into the cytosol and subsequent inhibition of caspase-3. These anti-apoptotic events were mediated through suppression of JNK and p38 MAPK signaling (Liu et al., 2017). Anti-inflammatory and anti-apoptotic effects by diosmin are also believed to decrease hypertension thus leading to an improvement of vascular problems. Treatment of patients with chronic venous insufficiency (CVI) with diosmin decreased free radical-induced cell damage and showed beneficial effects such as increased lymphatic drainage, microcirculation, capillary resistance, vascular tonus, and vein elasticity (Batchvarov et al., 2010; Feldo et al., 2018; Perrin and Ramelet, 2011). Noteworthy, the most significant changes in the alleviation of these CVI symptoms by diosmin were observed in smoker patients (Feldo et al., 2018). Animal models demonstrated neuroprotective effects by diosmin. In a mouse cerebral ischemia/reperfusion model, diosmin alleviated neurological deficits (Liu et al., 2014). A detailed analysis revealed anti-apoptotic signaling and an activation of JAK2/STAT3 pathways in animals treated with diosmin. Although the mechanisms leading to Alzheimer’s disease are only poorly understood, the pathology involves β-amyloid oligomerisation and tau-hyperphosphorylation. In a mouse model, an oral administration of diosmin reduced cerebral β-amyloid oligomer levels, tau-hyperphosphorylation and γ-secretase activity which resulted in cognitive improvement (Sawmiller et al., 2016).
The accumulation of free radicals released by immunocompetent cells in adipose tissue is considered to be a key pathologic link between obesity and type 2 diabetes. In a vicious cycle, reactive free radicals formed during chronic conditions of hyperglycemia and dyslipidemia are leading to insulin resistance resistance and pathological conditions of T2D (Bluher, 2016; Boutens and Stienstra, 2016; Calle and Fernandez, 2012; Chawla et al., 2011; Donath, 2014). In various models for diabetes, anti-diabetic effects of diosmin were demonstrated to be effective on different levels. Diosmin decreased oxidative stress as indicated by increased activities of antioxidant enzymes such as glutathione peroxidase and corresponding higher GSH levels as well as superoxide dismutase (Michael et al., 2013; Srinivasan and Pari, 2012). Anti-hyperglycemic effects were indicated by higher insulin sensitivity leading to declined levels of plasma glucose, HbA1c, reactive carbonyl species (RCS), and advanced glycation end products (AGEs) (Pari and Srinivasan, 2010; Patil et al., 2016). Lesser lipid peroxidation and reduced levels of triacylglycerols, free fatty acids (FFAs), cholesterol and LDL induced by diosmin demonstrated strong effects against dyslipidemia (Michael et al., 2013; Srinivasan and Pari, 2012; Srinivasan and Pari, 2013). These effects resulted in protection of diosmin against diabetic-induced damage of liver, kidney, eye and other organs as demonstrated in these studies.
In 1997, Tanaka and coworkers (1997b) found chemopreventive effects of diosmin against different cancers by the use of several rat models. In azoxymethane-induced colon cancer, the incidence and multiplicity of neoplasms (adenocarcinoma and aberrant crypt foci) were significantly decreased (Tanaka et al., 1997b). In another model, diosmin was effective in inhibiting the development of N-methyl-N-amylnitrosamine-induced esophageal tumorigenesis due to a suppression of cell proliferation in the esophageal mucosa (Tanaka et al., 1997a). In addition, the effects of diosmin against N-butyl-N-(4-hydroxybutyl)nitrosamine-induced urinary bladder carcinogenesis and 4-nitroquinoline 1-oxide-induced oral cancer were demonstrated to be based on decreased cell proliferation (Tanaka et al., 1997c; Yang et al., 1997). As observed for other flavonoids, an activation of apoptotic pathways by diosmin is considered to be responsible, at least in part, for its anticancer effects. In a prostate cancer cell line, free radical-induced genotoxic events and concomitant apoptotic cell death by diosmin were observed (Lewinska et al., 2015). Other pathways affected by diosmin leading to chemopreventive effects of diosmin might include receptor-dependent pathways. In MCF-7 human breast epithelial cancer cells, diosmin and diosmetin exhibited agonist activities on aryl hydrocarbon receptor (AhR), but only diosmetin was capable of inhibiting CYP1A1 enzyme activity, thus inhibiting carcinogenic activation (Ciolino et al., 1998).
In addition to studies performed with diosmin or diosmetin, several clinical studies have been conducted by the use of a micronized purified flavonoid fraction complex (Daflon®), consisting of 90% diosmin (450 mg) and 10% hesperidin (50 mg). Daflon® was launched for pharmacokinetic studies in France in 1971 for the treatment of chronic venous disease. Daflon® was well absorbed from the gastrointestinal tract, showed a very good tolerability, and exhibited therapeutic effects against CVI, venous leg ulcers and hemorrhoids (Hitzenberger, 1997; Struckmann, 1999). A recent systematic review and meta-analysis summarized the effectiveness of Daflon® by improving leg symptoms, edema and quality of life in patients with chronic venous disease (Kakkos and Nicolaides, 2018). In different in vitro and in vivo models, anti-inflammatory effects of Daflon® were demonstrated by reduced edema formation and leukocyte adherence, as well as attenuation of histamine, free radicals, prostaglandins and thromboxanes (Damon et al., 1987; Friesenecker et al., 1995; Jean and Bodinier, 1994; Lonchampt et al., 1989).
| 4. Conclusion and future directions | ▴Top |
In this review, we summarized current research on the use of rutin and diosmin, two major citrus fruit polyhydroxyflavones, as functional foods and therapeutic agents. Pharmacokinetic studies on bioavailability and biotransformation led to a better understanding of the biological activities executed by rutin and diosmin. Both flavone glycosides are hydrolyzed to their respective aglycones (e.g., quercetin and diosmetin for rutin or diosmin, respectively) during digestion by β-glucosidases. Quercetin and diosmetin are then rapidly absorbed by intestinal cells and converted to glucuronidated, sulfated, and methylated metabolites in further biotransformation reactions. Quercetin and diosmetin both showed strong potential as anti-disease chemopreventive or therapeutic agents. In a large number of cell-based in vitro, animal in vivo and human clinical studies, an impressive pharmacological profile with limited side effects has been demonstrated for quercetin. The pharmacological effects of quercetin were found to be pleiotropic on levels of free radical-scavenging, antioxidant, anti-inflammatory, antiproliferative and bioactivities to modulate apoptosis. Although many more studies were performed on rutin and quercetin, several studies demonstrated strong bioactivities also for diosmin and Daflon®, a combination of diosmin (90%) and hesperidin (10%). Emerging data from these studies suggest diosmin as being a promising candidate besides rutin for future therapeutic applications against degenerative diseases related to chronic inflammation.
| References | ▴Top |